May 26, 2021
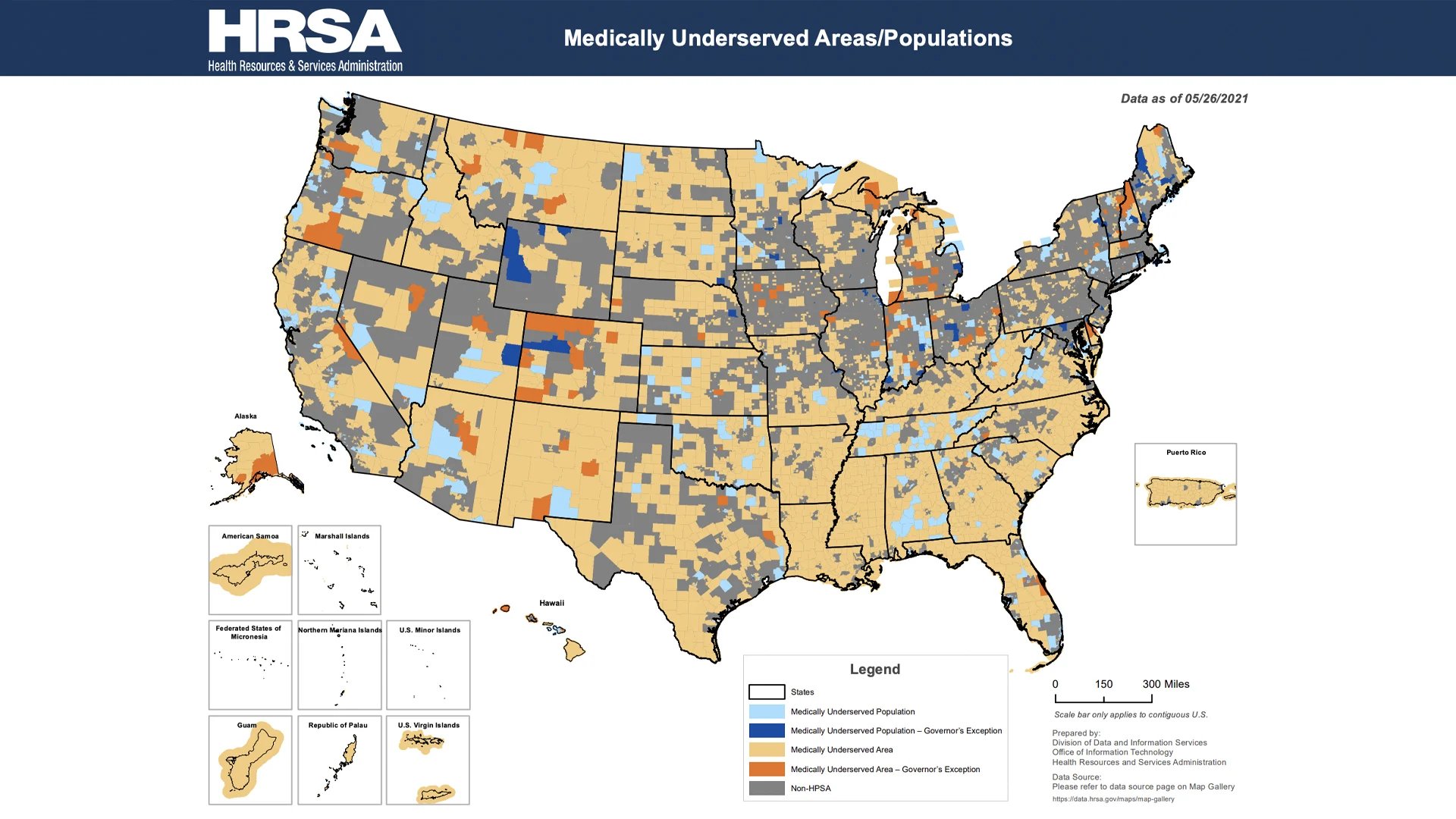
Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs) are organizations dedicated and funded to provide primary care services in medically underserved areas or populations. These programs provide primary care and ancillary services to individuals who are economically disadvantaged, in a medically underserved area or geographically isolated.
Currently there are over 12,000 FQHC sites and 4,500 rural health sites across the country.1 According to the HRSA, 1 in 12 people across the United States rely on FQHCs for care including 3.5 publicly housed patients, 1.4 million homeless patients, 1 million agricultural workers, and more than 355,000 veterans.2 RHCs facilitate 35.7 million visits per year and provide services for millions of people, including 8 million Medicare beneficiaries.3
Concert Health has partnered with community health centers in multiple markets to bring Collaborative Care – evidence-based behavioral health care – to patients who need it most. The Collaborative Care model integrates licensed behavioral health professionals in primary care to identify and treat patients with depression and anxiety.
Traditionally, 10-14% of patients on a primary care provider’s panel has a behavioral health need, an average that is often significantly higher in community health centers. The problem is exacerbated by a shortage of behavioral health providers to care for these patients, as health centers are often located in rural areas. The ability to bring evidence-based Collaborative Care to these high-need areas can impact entire communities.
- Concert Health has partnered with a total of six FQHCs and rural health centers in New York, Arizona and California, accepting just under 10,000 referrals for care.
- Of the over 150 providers in these centers, 76% of them have made at least one referral. Concert Health has served 2,875 patients and currently has 1,085 active patients.
- Many of these patients were high risk and flagged for suicide risk, 449 patients were removed from the suicide safer care pathway during treatment.
- Using a benchmark of a 50% of ten-point improvement in symptoms for depression and anxiety 44% patients met this benchmark in the first ninety days of care.
- FQHCs and rural health centers now have a new reporting measure, the number of patients who scored on the PHQ9 with depression and scored over 10 and who then had a subsequent score of 5 or less, of which 930 patients cared for met this goal.
The ability to expand behavioral health care, often in collaboration with internal embedded behavioral health providers, has allowed thousands of patients to access behavioral health care who otherwise would have had limited access. The addition of Concert Health and Collaborative Care has been paramount in helping health centers understand and manage populations of patients with behavioral health needs and meet quality measures and benchmarks.
Image credit: Health Resources and Services Administration (2021). Medically Underserved Areas/Populations. Retrieved from https://data.hrsa.gov/ExportedMaps/MapGallery/MUA.pdf
References:
- Centers for Medicare and Medicaid Services (2019). Rural Health Clinic Fact Sheet. Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/RuralHlthClinfctsht.pdf
- Definitive Healthcare (2019). How many Federally Qualified Health Centers are there? Retrieved from https://blog.definitivehc.com/how-many-fqhcs-are-there#:~:text=There%20are%20currently%201%2C368%20official,that%20number%20closer%20to%2014%2C200
- National Association of Rural Health Clinics (2018). About Us. Retrieved from https://www.narhc.org/narhc/ESX_About_Us_2.asp